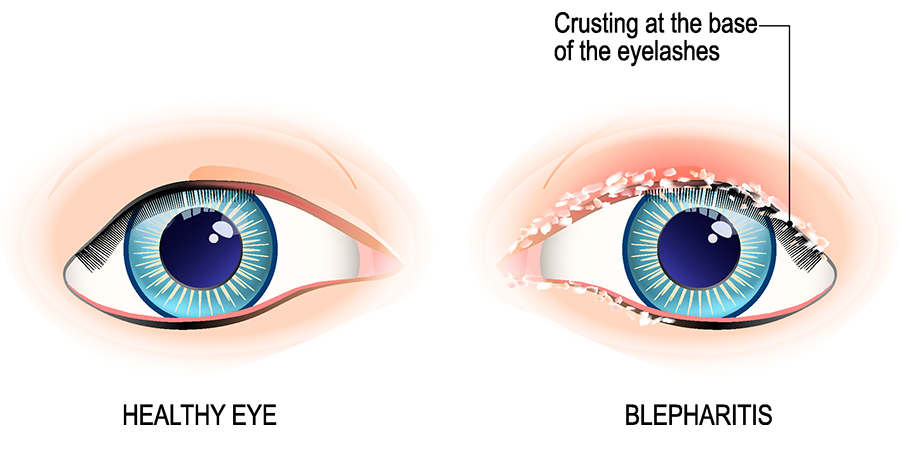
Blepharitis is a chronic inflammatory pathology of the free edge of the eyelids that develops with palpebral edema, ocular itching, hyper lacrimation, irritation and local burning sensation. Anterior blepharitis frequently develops with the appearance of scales at the level of the free edge of the eyelids, local erythema and edema. Posterior blepharitis is characterized by the loss of functionality of the Meibomius glands (sebaceous glands), their obstruction, the hypertrophy of the free edge of the eyelid and the formation of cysts at the level of the openings of the lacrimal glands.
How long does blepharitis heal?
What is chronic blepharitis?
Chronic blepharitis represents the most common form of evolution of this pathology, which is manifested by:
- Burning sensation
- Mild photophobia (sensitivity to light)
- The formation of crusts on the eyelashes and erythema of the free edge of the eyelids
- The local discomfort is more pronounced in the morning, the disease evolving with periods of remission and periodic exacerbations that cause the patient to go to the ophthalmologist for investigations and specialized treatment
Causes of blepharitis
The pathological mechanisms involved in the occurrence of blepharitis are incompletely defined, but it is considered that the etiopathogenesis of this condition includes a combination of the action of infectious factors of bacterial, viral, fungal or parasitic nature and the ability of the immune system to counteract these pathogens.
Bacterial infections are the main factor involved in the occurrence of blepharitis, there are numerous studies that confirm the destructive effect of pathogenic bacteria on the ecological balance of the ocular surface.
Staphylococcus aureus, S. epidermidis, Corynebacterium macginleyi and Propionibacterium acnes are the main microbial agents that generate the appearance of clinical manifestations associated with blepharitis. These bacteria were isolated by means of cultures of conjunctival secretions on special media in the microbiology department both in healthy people and in those with blepharitis. Under these conditions, it is suspected that these microorganisms have pathogenic potential (they become harmful and trigger infection) in certain favorable conditions, which allow their excessive development with the appearance of specific manifestations of blepharitis.
Risk factors of blepharitis
The main risk factors that predispose to the appearance of specific clinical manifestations of blepharitis are represented by:
- Uncorrected ametropia – vision deficiencies that cannot be corrected with eyeglasses, contact lenses or surgery
- Eye infections
- Exposure to dust
- The existence of an atopic terrain of the patient (predisposition to allergies)
- Diabetes mellitus
- Dry eye syndrome
- Humidity and low ambient temperatures
- Using expired or improperly stored cosmetics (dermatograph, mascara, mascara, blush, eye creams) and unsanitized make-up tools (eyelash curlers, mascara brushes)
- Inadequate palpebral tone (palpebral ptosis or drooping eyelid)
- Hormonal fluctuations
- Skin conditions: seborrheic dermatitis, rosacea acne
Blepharitis in children
The child’s blepharitis frequently manifests itself in the context of an evolving seborrheic dermatitis and is characterized by the presence of edema and erythema at the level of the eyelids that generate the appearance of small, dry and greasy crusts with scaly appearance.
The complicated evolution of blepharitis in children can be associated with conjunctivitis, chalazion or jugular.
Diagnosis of blepharitis
The diagnosis of blepharitis is established by the ophthalmologist with the help of the anamnesis, the clinical examination of the patient and the laboratory investigations represented by the culture of the conjunctival secretions to isolate the pathogenic germs involved in the occurrence of this pathology.
During the clinical examination, the ophthalmologist can collect scales from the base of the eyelashes for their microscopic examination to identify blepharitis caused by the presence of Demodex folliculorum or D.brevis at the level of the hair follicles.
In situations where there is suspicion of a parasitic infection at the eye level, the ophthalmologist can recommend the collection of hairs from the eyebrows or eyelashes to identify the cause that generates blepharitis.
In certain situations, conjunctival secretions can be processed by means of PCR molecular biology techniques in order to identify the genetic material of the microorganisms involved in the occurrence of blepharitis.
Blepharitis treatment
The treatment of blepharitis is etiological and aims to remove the causes that determine the appearance of the pathology and symptomatically to reduce the patient’s distressing manifestations.
Local hygiene at the level of the eyelids must be practiced rigorously during the administration of the treatment and involves the mechanical washing of their free edge with warm water and special soap, to remove impurities and reseal the openings of the lacrimal glands.
The daily massage of the eyelids improves the elimination of sebum and is practiced after proper hand hygiene or with the help of sterile compresses. The application of warm sterile compresses facilitates the detachment and removal of embedded secretions and scales from the eyelashes.
The etiological treatment is represented by antibiotic ointments with a bactericidal effect on the bacterial microorganisms involved in the occurrence of blepharitis. Topical corticosteroids are administered only on the recommendation of the ophthalmologist in accordance with the therapeutic scheme prescribed by him and must be used with caution for short periods, due to the side effects associated with these types of preparations.
Properly administered, cortisone-based ointments reduce the inflammation and itching associated with blepharitis. Depending on the severity of blepharitis and the presence of complications due to it, the ophthalmologist can prescribe the patient oral antibiotic treatment with different antibiotics depending on the susceptibility (sensitivity) of the pathogenic germ that generates the condition.
The tear film dysfunction associated with patients with dry eye syndrome can be corrected by applying artificial tears or obliterating the tear points by temporarily or permanently inserting special silicone plugs.
Wearing protective glasses against UV radiation and atmospheric particles prevents the occurrence of tear film dysfunction in patients with blepharitis, improving the symptoms associated with this pathology.
Cauterization of the lacrimal points is an irreversible method of stopping lacrimal hypersecretion reserved for patients unresponsive to other treatment methods for dry eye syndrome.
How long does blepharitis heal?
Therapy in the case of blepharitis tends to be long-term because the pathology frequently presents a recurrent character, associating periods of remission interrupted by exacerbations of symptoms.
The beneficial effects of the medication do not appear immediately, during the administration of the treatment, the patient needs careful monitoring for 3-4 weeks after the initiation of the specific therapy.
Untreated blepharitis
Chronic blepharitis, especially that of staphylococcal etiology, can evolve unfavorably with the thickening and scarring of the eyelid edges, the fall of the eyelashes and their deformation towards the cornea (trichiasis) which generates the sensation of a sting or foreign body in the eye and a state of permanent discomfort. Untreated blepharitis can cause complications represented by dry eye syndrome, chalazion, palpebral ulcers (of the eyelids) and blepharokeratoconjunctivitis, which can develop unfavorably with the appearance of eye infections or vision loss.
The main preventive measures for blepharitis include correct and periodic hygiene of the eyelids, avoiding the use of care cosmetics and eye makeup that has expired or incorrectly stored and shared with other people (even if they are family members), correct hand hygiene before applying lenses contact lenses and the use of protective glasses to avoid contact with dust and atmospheric allergens during outdoor activities.
Strict adherence to the treatment recommendations received from the ophthalmologist prevents relapses in patients with a personal history of blepharitis.
References:
- Classification of Chronic Blepharitis, James P. McCulley, Joel M. Dougherty, David G. Deneau
- Interventions for chronic blepharitis, Kristina Lindsley, Sueko Matsumura, Elham Hatef, Esen K. Akpek
- Medical management of blepharitis, Duncan, Katherine, Jeng, Bennie H, Current Opinion in Ophthalmology